Throughout the years, body augmentation has become increasingly popular. In fact, breast implants continue to be the most popular procedure done by plastic surgeons. In 2017, 290,467 people underwent surgery for breast implants, and that number has undoubtedly continued to remain high [1]. This means that more and more women with breast implants are questioning whether they can breastfeed their babies.
Can you breastfeed with implants? Is it safe? What complications should you expect? Read on for the answers to these questions and more.
Breastfeeding With Implants: Can It Be Done?
First, if you have breast implants, you should know that you can breastfeed—but it is never guaranteed. The possibility depends on a couple of factors, such as the type of breast implant you have, the placement, and the surgical techniques that were used. You may also need to worry about chemicals from the implants leaking into your breastmilk [2].
However, that usually only applies to silicone implants. If you have saline water implants, there are no adverse effects.
Another question that is often asked is whether breastfeeding with implants is safe. Currently, there are gaps in knowledge and conflicting views that prevent a firm yes or no. For the most part, we know that silicone is inert, or chemically inactive, so even if it leaks into breastmilk, the gastrointestinal tract is not likely to absorb it. Other research has hinted to silicone causing some inflammation in the body, but there have been no long term studies to see how this would affect a baby, if at all.
If you are concerned about the health impacts of breast implants, you may want to do your own supplemental research, since it goes beyond the scope of this article.
What Problems Should I Expect During Breastfeeding With Implants?
There are a few challenges you should anticipate:
- Low milk production. Depending on the kind of surgery you had done, you could have trouble making enough milk to breastfeed exclusively. You may need to supplement with formula. Research has found that women with breast implants are three times as likely as women without augmentation to have decreased milk supply.
- Inhibited letdown. Sometimes, your nipples may have lost sensitivity, or you have scar tissue within the breasts, that will lessen the letdown reflex. Again, this lowers milk production.
- Painful nipples. Some women develop high sensitivity in the nipples, which can make nursing more painful than usual.
- Breast engorgement. Women with breast implants are far more likely to experience painful engorgement more often. If milk doesn’t drain completely from the breast, it can get stuck in the breast, creating blisters, bleps, engorgement, and even infection.
- Mastitis. The risk of mastitis, an infection of the breast tissue, is increased due to implants.
A quick note about a letdown. The incision made during the surgery can affect it. The areola is more than just dark skin. It has thousands of nerve endings that are connected to the letdown effect. Whenever your baby begins to suckle on the breast, the nerves are invigorated and send signals to the brain to increase the levels of oxytocin and prolactin. Oxytocin tells the body to release milk, while prolactin starts the production of breastmilk.
At any time you have scarring or inhibited letdown, you will have issues making enough milk.
Will Breastfeeding Ruin My Implants?
No, breastfeeding will not affect your implants. The appearance of augmented breasts should remain the same, especially if given enough time to heal before breastfeeding.
Effects on Milk Production
Will your milk supply be affected by breast implants? Probably. Fortunately, even if the surgery has damaged the mammary glands of the breasts, where the milk is made, you should still be able to produce breastmilk. Even the smallest quantity is better than nothing.
Here are some ways implants may affect milk production:
- Incision type and placement. Some techniques (mentioned in more detail below) can damage milk ducts, the mammary glands, and nerves more than other methods. Additionally, incisions made around the dark skin surrounding the nipple, the areola, may cut into ducts and nerves that assist with breastfeeding.
- Under the breast incisions. If you had an incision under the breast, where the breast meets the chest, then you have some damage to nerves and ducts. While these nerves will repair themselves, it may take a while. Generally, the longer time between your breast augmentation and pregnancy, the less damage you have to worry about.
- Implant placement. Implants are either placed under or over the muscle in the breasts. When they are placed over, there is more pressure on the glandular tissue and milk ducts, thus slowing milk production.
- Numbness. Sometimes, breast implants will result in nerve damage that causes numbness (or pain). Scarring deep in the ducts may not heal and will cut off milk supply.
- Reasons for surgery. If you got surgery because of hypoplastic (underdeveloped) breasts, you will probably have trouble producing enough milk. Remember, just because the implants make you look bigger, the functional components are unchanged. Women who usually have less functional tissue have naturally wide-spaced breasts, asymmetrical breasts, or tube-shaped breasts.
- Date of surgery. It can take up to two years for nipple sensation to return. Plus, many breast implants require revision, which can cause further damage to the breast tissue and milk ducts, increasing the risk of poor milk production.
Lastly, complications that arise from breast implants also need to be considered. Since breast implants are not considered a lifetime device and will sometimes need corrective surgeries, the chance of complications rises. Complications from breast augmentation include hardening of the breast tissue around the implant, long-term pain, surgical removal of painful scar tissue, required changes in size of the implant, repeated uplifts, and pressure caused by infection. All of these things can later affect lactation.
Tips For Breastfeeding With Implants
Even a little breastmilk can benefit your baby. Here are some ways to help nursing with implants:
Breastfeed as often as possible.
Ideally, you want to breastfeed around 8-10 times a day. This will establish a routine with your baby and also maintain the milk supply. When your baby suckles, it promotes a natural reaction that directs your breasts to lactate. The more often you feed your baby or use a breast pump, the more milk you create.
Remember, you might not be able to produce a lot, but even the little amount you produce will be beneficial. Your baby will receive antibodies, vitamins, and minerals from breastmilk. Be sure to use both breasts when breastfeeding, as well.
Also, if you had damaged ducts, nerves, or glands after the augmentation, you should attempt breastfeeding. Glandular tissue is known to develop in the presence of breastfeeding hormones. Plus, areas of the breast that were undamaged can compensate for the damaged regions. Even if you struggle to produce milk during your first pregnancy, a second pregnancy may result in much greater milk production.
Empty your breasts throughout the day.
One of the most important parts of milk production is to empty your breasts as often as you can. This will not only accelerate milk production but will prevent breast engorgement and mastitis, both of which are a risk of breastfeeding with implants.
Try manually expressing breastmilk or using a pump throughout the day and even after feedings. The increased demand for breastmilk will signal to your body to produce more milk.
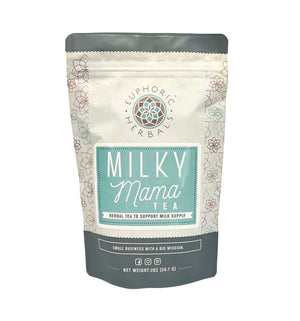
Use galactagogues.
You may have heard about galactagogues before. These are natural herbs that can increase your breast milk production. This includes:
- Fenugreek
- Milk thistle
- Fennel
- Nettle
- Ginger
Oftentimes, you can find herbal tea blends designed with these galactagogues. You can also try lactation cookies, which can be purchased online or even homemade. Lactation cookies usually contain ingredients known to support female health, such as wheat germ, whole wheat, flaxseed, and herbal galactagogues.
Other galactagogues include:
- Carrots, beets, yams
- Leafy greens, like kale, spinach, and collard greens
- Green papaya
- Nuts
- Chickpeas
- Sesame seeds
However, it is recommended that before you try a galactagogue that you discuss it with a medical professional. Some herbs will interact with prescription medications and may have adverse effects.
How To Help Your Baby Latch Correctly
Because breast implants can augment the position of the nipple, you may have to work on getting a correct latch. You can do this by helping your baby move their head into the right position. Hold the nape of their neck gently. You can also touch their top lip with the nipple, prompting them to open their mouth then guide the nipple in. Also, look at the positioning of their mouth when holding the nipple. The lower lip and chin should be touching the areola—the dark ring around the nipple.
How To Tell If Your Baby Has a Correct Latch
Here are some things to look for to ensure your baby is latched on:
- You can hear your baby swallowing milk
- They are relaxed and taking slow mouthfuls
- Your nipple doesn’t hurt when nursing
- Your nipple is the same shape after your baby finishes breastfeeding
- Your baby can start suckling immediately
- The nipple is smooth, showing no dimples or wrinkles from where the baby had latched on
How Do I Know I’m Making Enough Milk?
Since breast implants may compromise your milk production, you may want to make sure that your baby is getting enough milk. The general way to gauge this is by the number of diapers you go through. 3-4 bowel movements and 6-8 wet diapers are the average per day for a well-fed baby.
You can also consider how much milk you need to express after feeding. If you are manually expressing or pumping and not getting much extra, you may be experiencing low milk production. Again, you can try to increase breastmilk production by consuming some herbal teas or lactation cookies, but you may want to supplement with infant formula in the meantime.
Should I Supplement With Formula?
In the event your baby is not getting enough milk, you will notice that they are not gaining any weight. You should discuss options with your doctor or a lactation consultant about supplementing with formula. There are other ways to increase your milk supply, however, so you should do some research to see which method is best for you.
Other reasons you should discuss supplementing with formula include:
- Failing to produce milk within 5 days of delivery
- Your baby is producing less than 6 wet diapers or 3 bowel movements (or both)
- Your baby nurses less than 8 times a day
- You experience nipple pain during or between breastfeeding
Takeaway
While breastfeeding with implants can increase difficulties, you can still be successful. Breastfeeding also won’t ruin your implants. Work closely with medical professionals or lactation consultants, feed your baby often, use a breast pump, and supplement with baby formula if necessary. Remember to discuss your implant surgery with your doctor as well.
Have more questions about breastfeeding that weren’t answered here? Want updates? Then fill out the contact form to get more info sent to your inbox.